The U.S. Food and Drug Administration (FDA) has removed its long-standing “black box” warning from more than 20 hormone-based menopause drugs, including pills, patches, and creams containing estrogen and progestin. The agency said Monday that the change reflects modern medical understanding of hormone therapy risks and benefits.
The warning, first introduced 22 years ago, cautioned that hormone replacement therapy could raise the risk of heart disease, stroke, blood clots, dementia, and certain cancers. The FDA now says newer evidence indicates that these risks are far lower when the treatment is prescribed before age 60 or within 10 years of the onset of menopause.
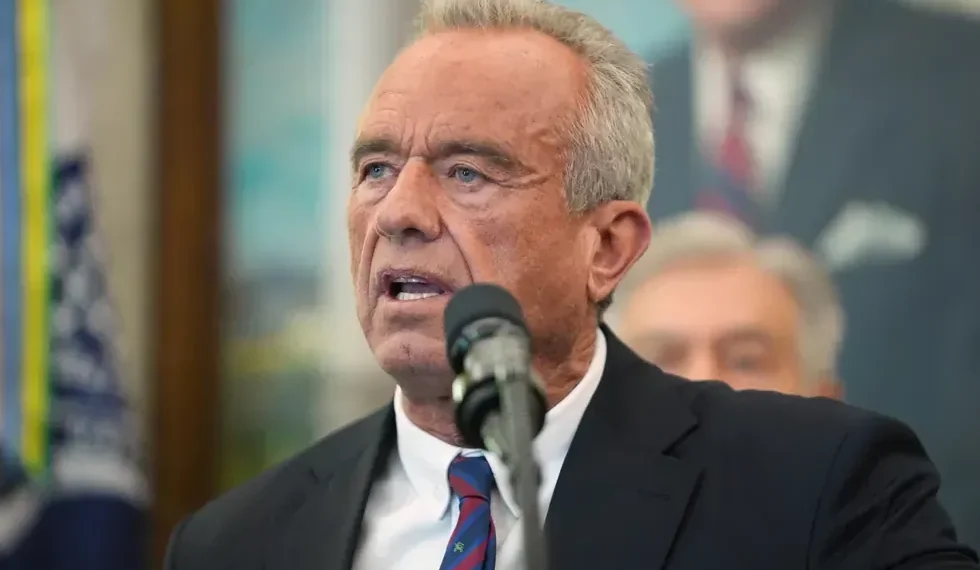
“We’re challenging outdated thinking and recommitting to evidence-based medicine that empowers rather than restricts,” said Health Secretary Robert F. Kennedy Jr. during the announcement.
The revision affects widely used therapies intended to ease symptoms such as hot flashes, night sweats, and mood changes—conditions that affect millions of women during menopause.
Updated Guidelines Reflect Evolving Science
FDA Commissioner Dr. Marty Makary, who has long advocated for removing the warning, called the previous label “outdated and unnecessary.” He said the decision aligns with findings from recent studies showing that hormone therapy can be safe and beneficial for many women when used appropriately.
“With few exceptions, there may be no other medication in the modern era that can improve women’s health outcomes at a population level more than hormone replacement therapy,” Makary told reporters.
The agency’s updated prescribing information now aligns with modern medical guidelines, which recommend using hormone therapy for a limited duration among younger women without complicating risk factors such as breast cancer or blood clotting disorders.
Still, not all experts agree. Dr. JoAnn Manson of Harvard Medical School said that while removing the warning was “a good step toward personalized care,” the benefits described by Makary are “not as conclusive or definitive.”
“The black box is really one size fits all—it scares everyone away,” Manson explained. “Without it, there can be more focus on how the risks and benefits differ by age and health profile.”
A Shift from Two Decades of Caution
The FDA’s original boxed warning was based on findings from the landmark Women’s Health Initiative (WHI) study, published in 2002, which linked hormone therapy to higher rates of heart disease, blood clots, and breast cancer.
The study, involving over 26,000 women, led to a dramatic decline in hormone therapy prescriptions across all age groups. In the 1990s, roughly one in four American women used estrogen-based treatments, often believing they could prevent heart disease and dementia.
However, later analyses of the WHI data have revealed more nuanced results. A new review published in September found that women in their 50s taking estrogen-based drugs did not face an increased risk of heart problems, while risks were higher for those in their 70s. For women in their 60s, the data remained inconclusive.
“These findings suggest that timing and age at initiation make a significant difference in outcomes,” said Dr. Steven Fleischman, president of the American College of Obstetricians and Gynecologists. “The old warning scared patients away even when hormone therapy might have helped them.”
Fleischman added that many women stopped seeking treatment altogether after reading the label. “I can spend 30 minutes counseling someone about hormone therapy, but when they see that warning, they just get scared,” he said.
FDA’s Review Process Sparks Criticism
Despite widespread support from some physicians, the FDA’s approach to revising the warning has drawn criticism from several health policy experts who argue that the agency bypassed its usual advisory process.
Typically, the FDA consults independent advisory committees when revising safety labels. Instead, Makary convened a smaller, informal panel of about a dozen doctors and researchers—many of whom publicly advocate for hormone therapy or have ties to pharmaceutical companies that manufacture these drugs.
Diana Zuckerman, president of the nonprofit National Center for Health Research, said the decision risks undermining public trust. “By skipping a formal scientific meeting and instead holding a news event, the FDA appears to have prioritized messaging over transparency,” she said.
Makary defended the move, arguing that advisory committee meetings are “bureaucratic, long, often conflicted, and very expensive.”
New Labeling Still Includes Cancer Advisory
Although the FDA has removed the broader black box warning, the updated labels will still contain a boxed notice advising that women who have not had a hysterectomy should take a combination of estrogen and progestin to reduce the risk of uterine cancer.
The older warning language will remain on the label but appear in a less prominent section.
Additionally, the market has evolved since the early 2000s, with newer formulations delivering hormones in lower doses and through localized delivery systems such as vaginal creams and tablets. These methods limit how much hormone circulates through the bloodstream, potentially lowering systemic risks.
Ongoing Debate Over Hormone Therapy’s Role
The controversy over hormone therapy reflects broader debates in women’s health about how medical evidence is interpreted and communicated. Advocates say the FDA’s decision could help reduce stigma and make more women comfortable discussing treatment options. Critics warn that downplaying risks could lead to overprescription.
Medical experts emphasize that hormone therapy should be prescribed on an individual basis, taking into account age, health history, and symptom severity.
“The removal of the black box is not a green light for everyone,” Dr. Manson noted. “It’s an invitation to nuanced, evidence-based decision-making.”
As hormone therapy reenters public conversation, researchers say long-term studies are still needed to confirm whether the treatment can truly reduce the risk of chronic conditions like Alzheimer’s and heart disease—claims that remain scientifically unsettled.
This article was rewritten by JournosNews.com based on verified reporting from trusted sources. The content has been independently reviewed, fact-checked, and edited for accuracy, neutrality, tone, and global readability in accordance with Google News and AdSense standards.
All opinions, quotes, or statements from contributors, experts, or sourced organizations do not necessarily reflect the views of JournosNews.com. JournosNews.com maintains full editorial independence from any external funders, sponsors, or organizations.
Stay informed with JournosNews.com — your trusted source for verified global reporting and in-depth analysis. Follow us on Google News, BlueSky, and X for real-time updates.