Measles Outbreaks: Lessons from the Past and Challenges Ahead
The Battle Against Measles: Then and Now
Six years ago, the United States faced its worst measles outbreaks in decades. Two communities in New York—Brooklyn and Rockland County—were at the center of this crisis, bringing the country dangerously close to losing its measles elimination status, which had been achieved in 2000.
Today, similar outbreaks are unfolding in West Texas and New Mexico, prompting urgent action. Testing sites and vaccine clinics have been set up, and the US Centers for Disease Control and Prevention (CDC) has stepped in to assist. However, local health officials warn that the spread could continue for months.
A Coordinated Response in 2019
The 2019 measles outbreaks in New York were met with swift and sustained public health efforts. These responses were tailored to the affected communities, combining direct engagement with formal policy changes. Experts emphasize that this comprehensive approach is crucial for containing current and future outbreaks.
The Power of Vaccination
The outbreaks in New York were concentrated in Orthodox Jewish communities that had been exposed to years of anti-vaccine disinformation. Public health officials focused on building trust within these communities to encourage vaccinations—the most effective tool against measles.
“Vaccination is the most important way to prevent the devastating disease that measles can be,” said Dr. Neil Vora, executive director of Preventing Pandemics at the Source.
The measles vaccine is highly effective—two doses provide 97% protection—and long-lasting. Because measles is extremely contagious, a 95% vaccination rate is needed to prevent outbreaks.
During the 2019 outbreak, more than 200,000 doses were administered in New York City and 30,000 in Rockland County, significantly boosting immunization rates. However, overcoming vaccine hesitancy took time.
Dr. Oxiris Barbot, former New York City health commissioner, noted that the persistence of disinformation made it difficult to achieve rapid vaccination rates. “That’s why it’s so important to rely on trusted messengers,” she emphasized.
New York City’s strong vaccine registry played a key role in identifying at-risk individuals and streamlining vaccination efforts. Other regions facing outbreaks may struggle due to limited resources.
Reaching Communities One Household at a Time
Public health workers took an individualized approach, going door-to-door and answering vaccination concerns directly. In some cases, people were vaccinated discreetly to avoid social backlash.
This hands-on effort helped curb the outbreak. A retrospective study found that New York City’s vaccination campaigns prevented a much larger crisis—potentially 8,100 cases instead of the reported 649.
The Danger of Misinformation and Community Transmission
While increasing vaccination rates was crucial, other factors also played a role. Some community-organized “measles parties,” intended to spread the virus deliberately, accelerated transmission. Infants were particularly vulnerable, as they were too young to be vaccinated.
By late 2018, more than half of infants in affected communities were susceptible to measles, along with a quarter of children aged 1-4. Although vaccination campaigns initially slowed the outbreak, by early 2019, transmission rates spiked, likely due to increased close-contact exposure among children.
Policy and Emergency Declarations
In April 2019, New York City and Rockland County declared a state of emergency. These declarations provided essential resources for outbreak control and reinforced public health mandates.
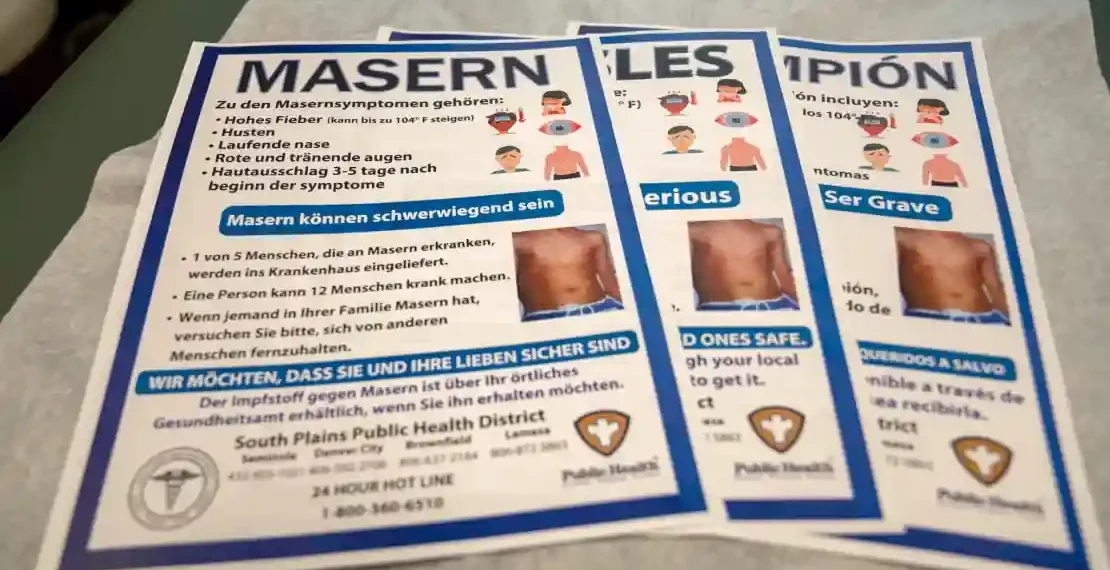
However, formal policies were only part of the solution. Trusted community leaders played a critical role in dispelling misinformation and encouraging vaccination. Dr. Blima Marcus, a nurse practitioner and member of the Orthodox Jewish community, developed culturally tailored informational materials, reaching thousands of households.
“The only thing that can truly help is when a community mobilizes from within,” Marcus said. “Knocking on doors—literally and figuratively—helps change the narrative.”
Comparing Past and Present Outbreaks
By the time the 2019 outbreaks ended, Rockland County had reported 312 cases and New York City 649. Fortunately, no deaths occurred.
The current outbreaks in Texas and New Mexico, however, have already resulted in nearly 230 cases and two deaths. Much of the spread is occurring within a Mennonite community, which, like the Orthodox Jewish communities in New York, faces vaccine hesitancy challenges.
Marcus stressed that cultural competence is key to public health outreach. “People resist being told what to do by outsiders who don’t understand their beliefs,” she explained.
Looking Forward
The lessons from the 2019 outbreaks highlight the need for proactive, community-centered strategies. Vaccination remains the strongest defense against measles, but public health efforts must also address misinformation and cultural concerns.
As the current outbreaks evolve, an all-hands-on-deck approach—combining medical expertise, community engagement, and policy support—will be essential to containing the spread and protecting vulnerable populations.
This article was rewritten by JournosNews.com based on verified reporting from trusted sources. The content has been independently reviewed, fact-checked, and edited for accuracy, neutrality, tone, and global readability in accordance with Google News and AdSense standards.
All opinions, quotes, or statements from contributors, experts, or sourced organizations do not necessarily reflect the views of JournosNews.com. JournosNews.com maintains full editorial independence from any external funders, sponsors, or organizations.
Stay informed with JournosNews.com — your trusted source for verified global reporting and in-depth analysis. Follow us on Google News, BlueSky, and X for real-time updates.